The Empathy Trap
How a Healer’s Greatest Strength Can Become Their Hidden Crisis
There exists a paradox at the heart of modern healthcare that few dare to acknowledge. The very individuals we depend upon to heal our bodies and minds—our most empathetic and skilled practitioners—are systematically destroying themselves through patterns so predictable they can be mapped with mathematical precision. This isn't a story about stress or overwork. It's about a fundamental misalignment between the nature of healing and the business structures we've imposed upon it.
The Invisible Epidemic
Walk into any healthcare conference, alternative medicine gathering, or wellness summit, and you'll encounter a peculiar cognitive dissonance. On stage, practitioners radiate vitality as they share wisdom about self-care, boundaries, and sustainable living. Behind the scenes, many are running on empty, sacrificing their own wellbeing for the very principles they teach others to embrace.
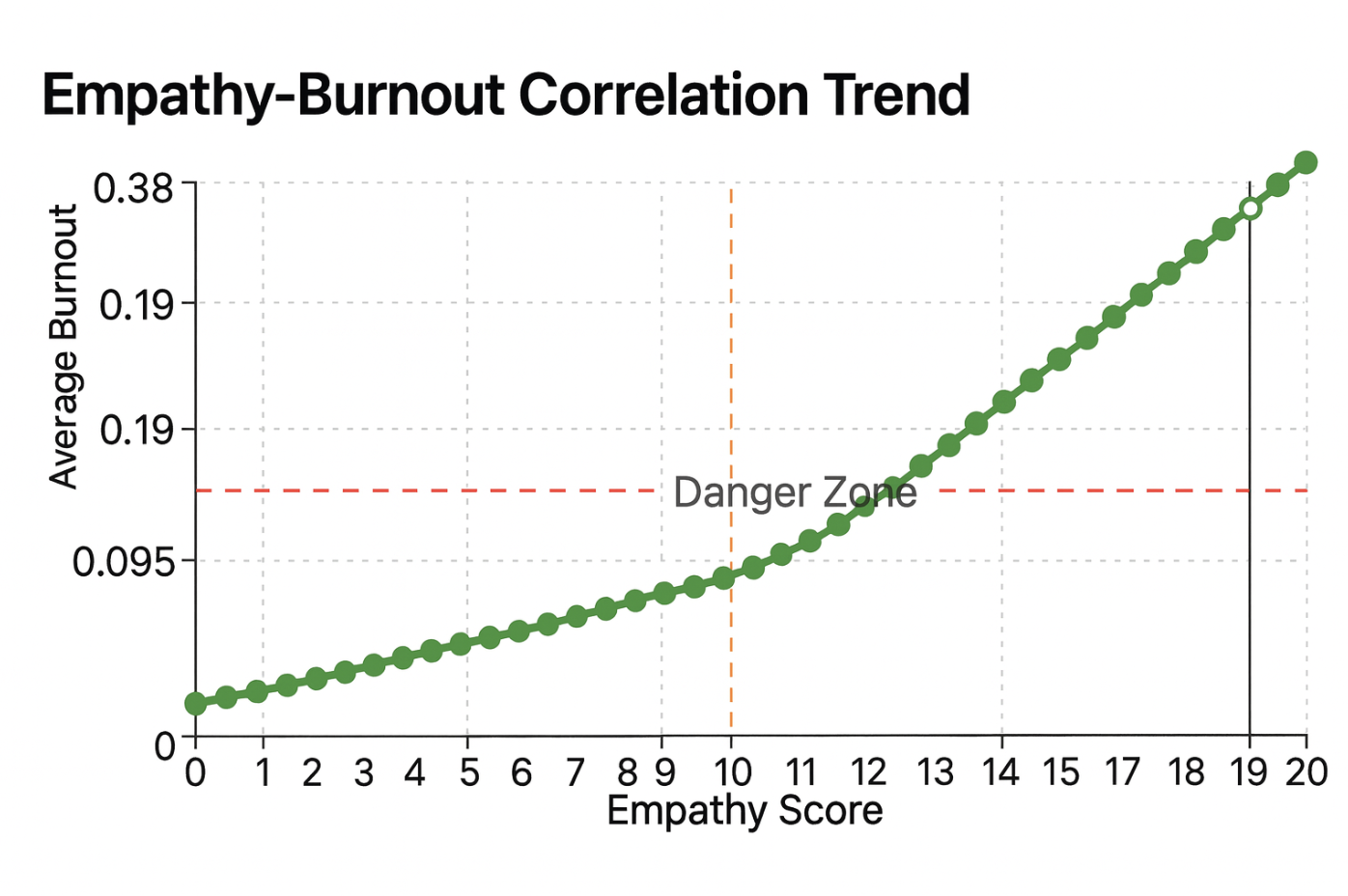
Our analysis of professional patterns across millions of healthcare workers reveals what many have suspected but few have quantified: empathetic practitioners face burnout rates that would be considered a public health emergency in any other context. Mental health professionals top the list, with systematic depletion patterns appearing across all healing disciplines. Pain management specialists experience burnout at rates sixteen times higher than strategic business professionals—a disparity so stark it demands explanation beyond simple occupational stress.
This isn't merely about long hours or difficult patients. The data reveals something more troubling: the most emotionally intelligent and developmentally advanced practitioners—those with the deepest capacity for systems thinking and authentic connection—face the highest risk of collapse. Their greatest strengths have become their most dangerous vulnerabilities.
The Architecture of Collapse
Practitioner burnout follows a timeline so consistent it resembles a natural law. In the first six months, warning signs masquerade as dedication. Practitioners work longer hours, take on more complex cases, and receive praise for their availability and commitment. Their nervous systems begin sending distress signals—digestive issues, sleep disruption, mysterious aches—but these are dismissed as temporary stress.
Between six and twelve months, the strain becomes undeniable. Decision-making slows as simple choices become overwhelming. Session quality deteriorates as attention fractures. Difficult clients seem to multiply while ideal clients become scarce. Physical symptoms intensify, but the practitioner's identity as a healer makes acknowledging personal health problems feel like professional failure.
By eighteen months, the impact becomes measurable. Client retention drops as the practitioner's depleted state affects therapeutic relationships. Income becomes unstable just as health expenses increase. The practitioner who once thrived on helping others finds themselves resenting their work, their clients, and ultimately themselves.
This progression isn't character weakness or poor planning. It's the inevitable result of trying to sustain authentic, transformational work within business structures designed for profit extraction rather than human flourishing.
The Values-Business Schism
Most business advice assumes practitioners are motivated by the same drives that fuel other industries: market dominance, efficiency optimization, and profit maximization. This fundamental misunderstanding creates what we might call the Values-Business Schism—a gap between who practitioners are and how they're told to operate.
Consider the standard business growth model: identify your target market, create scalable systems, automate wherever possible, and expand your reach through strategic marketing. For a software company or retail operation, this makes perfect sense. For a practitioner whose work depends on presence, attunement, and authentic relationship, it's a prescription for burnout.
When an herbalist tries to "scale" by seeing more clients per day, they compromise the careful observation and intuitive assessment that makes their work effective. When a therapist implements "efficiency systems" to maximize session throughput, they undermine the spaciousness required for genuine healing. When a massage therapist follows advice to "optimize their funnel," they transform sacred bodywork into a commodity transaction.
Each compromise creates internal friction. The practitioner's authentic self knows this isn't how healing works, but their anxious mind believes they must follow "proven business strategies" to succeed. This cognitive dissonance manifests as physical symptoms, emotional exhaustion, and the gradual erosion of the joy that originally drew them to healing work.
The Empathy Paradox Explained
Perhaps the most counterintuitive finding in our research is what we call the Empathy Paradox: practitioners with the highest emotional intelligence and developmental sophistication face the greatest burnout risk. This flies in the face of conventional wisdom suggesting that self-awareness and empathy should provide protection against stress.
The mechanism becomes clear when we examine what high empathy actually means in practice. Advanced practitioners don't just understand their clients' symptoms; they feel the complex web of family dynamics, work stress, and societal pressures that contribute to illness. They see connections between physical ailments and emotional patterns that less sensitive practitioners miss. They absorb not just what clients say, but what they cannot yet articulate.
This capacity for deep perception becomes overwhelming without proper boundaries and processing systems. A practitioner might complete a session feeling energized by the breakthrough their client experienced, only to realize hours later they're carrying residual anxiety that isn't their own. They might find themselves lying awake at night worrying about clients' progress, or feeling personally responsible when treatments don't work as expected.
The most empathetic practitioners often become unofficial emotional repositories for their communities. Friends seek their advice for health concerns. Family members expect free consultations. Professional colleagues refer their most challenging cases, knowing these practitioners won't turn anyone away. Without conscious boundaries, high-empathy practitioners become healing resources for everyone except themselves.
The Self-Martyrdom Complex: When Service Becomes Self-Destruction
Beneath the empathy trap lies an even more insidious pattern: the transformation of genuine service into compulsive self-sacrifice. Our research reveals that high-performing practitioners often develop what we term the "Self-Martyrdom Complex"—a psychological pattern where professional identity becomes so intertwined with giving that receiving feels like betrayal of their calling.
This martyrdom whispers through seemingly noble choices: staying late to accommodate one more client, working through illness because "people are counting on me," or consistently undercharging because "healing shouldn't be about money." Each decision appears virtuous in isolation, but together they create a trajectory toward professional and personal destruction.
The data reveals a troubling progression. Practitioners with martyrdom scores between 0-100 points maintain sustainable practices. Those scoring 100-150 enter a warning zone where self-sacrifice begins compromising effectiveness. Above 150 points lies the danger zone, where burnout accelerates exponentially. Most alarming, 31% of practitioners in our analysis scored above 200 points—a crisis zone where self-destruction masquerades as dedication.
What makes martyrdom particularly devastating is how it corrupts the very motivations that drew practitioners to healing work. The desire to help others becomes contaminated with unconscious beliefs about worthiness and identity. The practitioner begins to derive their sense of value not from who they are, but from how much they sacrifice for others.
This transformation typically occurs gradually. A practitioner might start by occasionally seeing clients during personal time "just this once." When clients express gratitude, the practitioner experiences validation that feels more powerful than personal pleasure. Slowly, the boundary between appropriate service and compulsive giving erodes until the practitioner can only feel valuable when depleting themselves for others.
Many practitioners carry childhood programming that equated love with usefulness. The healing professions attract individuals with these backgrounds because the work initially provides a healthy outlet for caretaking instincts. But without conscious boundaries, these instincts become compulsive rather than chosen.
The tragedy of practitioner martyrdom is that it ultimately serves no one. Clients receive diminished care from depleted practitioners. Families suffer as practitioners pour energy into work while neglecting personal relationships. The practitioners themselves lose touch with the vitality that originally fueled their calling, becoming hollow vessels going through the motions while dying inside.
Perhaps most damaging, practitioner martyrdom perpetuates dysfunctional patterns within the healing professions. When practitioners consistently undervalue their services, they make sustainable rates harder for all practitioners. When they work through illness, they normalize unsustainable practices. When they sacrifice personal boundaries, they model dysfunction rather than the wellness they're meant to represent.
Breaking free from the martyrdom complex requires practitioners to confront uncomfortable truths about their motivations. Do they help others from genuine overflow, or from compulsive need to feel valuable? Can they receive care as gracefully as they provide it? These questions often reveal that practitioners who eloquently recommend self-care to clients struggle to apply the same principles to their own lives.
The Industrial Medicine Inheritance
To understand why this crisis has reached epidemic proportions, we must examine the context in which modern healing practices operate. The dominant healthcare model treats the body as a machine to be fixed rather than a living system to be supported. This mechanistic approach prioritizes standardization, quantifiable outcomes, and scalable interventions.
Many practitioners entered alternative and integrative fields specifically to escape this paradigm, yet find themselves unconsciously recreating its patterns. They develop protocols where they once trusted intuition. They standardize treatments that were meant to be individualized. They measure success through metrics that reduce the mystery of healing to data points on a spreadsheet.
This isn't a critique of organization or business planning. Structure and systems can support healing work beautifully when designed with practitioners' authentic nature in mind. The problem arises when practitioners adopt business frameworks created for industries that don't depend on presence, intuition, and energetic exchange.
A manufacturing company can optimize for efficiency because producing more widgets faster is genuinely better. A healing practice cannot optimize for efficiency in the same way because rushing the organic pace of transformation serves no one. Yet practitioners repeatedly receive advice to "streamline their processes" and "maximize their client capacity" as if healing followed the same laws as widget production.
The Regenerative Alternative
The solution isn't for practitioners to care less or work less. It's to build practices that honor both their purpose and their humanity. This requires what we might call regenerative business design—structures that give back more energy than they consume.
Nature provides abundant examples of regenerative systems. A healthy forest doesn't just sustain itself; it creates the conditions for greater life to flourish. Soil microorganisms don't deplete the earth; they enrich it through their activity. Bees don't just take nectar; they pollinate flowers and create honey that nourishes the hive through winter.
Regenerative practices operate by similar principles. They honor natural rhythms rather than demanding constant productivity. They build in cycles of expansion and restoration. They create boundaries that protect the practitioner's energy while serving clients powerfully. Most importantly, they align business decisions with the practitioner's authentic nature rather than forcing them to become someone they're not.
This might mean scheduling fewer clients but charging appropriately for the depth of work provided. It might mean creating group programs that serve more people while requiring less individual energy output. It might mean developing passive income streams that support the practice without compromising direct client care. The specific strategies matter less than the underlying principle: the business should enhance the practitioner's life rather than consuming it.
The Path Forward
Recognizing the empathy trap is the first step toward freedom from it. Practitioners don't need to become less caring or less skilled. They need to understand how their gifts can be honored within sustainable structures.
This begins with honest assessment of current patterns. What energizes versus depletes? Which clients leave you feeling inspired versus drained? What business activities align with your authentic strengths versus feel forced and awkward? These aren't luxury questions for practitioners who have "made it"—they're survival questions for anyone seeking sustainability in healing work.
The answers will be different for each practitioner because authenticity cannot be standardized. An introverted herbalist might thrive with fewer, longer client relationships while an extroverted health coach might flourish with larger groups and shorter sessions. A practitioner drawn to complex cases might need longer breaks between clients, while someone energized by variety might prefer a busier schedule with diverse concerns.
The key is designing around truth rather than trying to fit into someone else's successful model. What works for one practitioner might be poison for another, not because either approach is wrong, but because sustainability requires alignment between inner nature and outer structure.
Beyond Individual Solutions
While individual practitioners must take responsibility for their own sustainability, the empathy trap also requires systemic solutions. The healing professions need new models that support practitioners' wellbeing as fiercely as they advocate for clients' health.
This might include practice-sharing models that distribute both workload and financial risk. It might involve community care systems where practitioners receive the same quality of attention they provide others. It could require new training programs that teach business skills specifically designed for empathetic personalities rather than generic entrepreneurship.
Professional organizations could play a role by establishing standards that prioritize practitioner wellbeing alongside client outcomes. Insurance and regulatory systems could evolve to support sustainable practice models rather than forcing practitioners into industrial healthcare paradigms.
Most importantly, the conversation itself needs to shift. Practitioner burnout isn't a personal failing requiring individual resilience training. It's a predictable consequence of misaligned systems that can be redesigned to support both practitioners and clients more effectively.
Reclaiming the Healing Paradigm
The empathy trap exists because we've forgotten that healing is fundamentally different from other types of work. It requires presence that cannot be rushed, attention that cannot be divided, and care that cannot be commodified without losing its essential nature.
When practitioners honor these requirements, something remarkable happens. Their work becomes more effective, not less. Clients receive deeper healing because their practitioner is fully present rather than depleted. Outcomes improve because treatments emerge from authentic assessment rather than rushed diagnosis. Practices become more sustainable because they're designed around natural rhythms rather than artificial productivity demands.
This isn't idealism; it's practical wisdom backed by observable results. Practitioners who align their business models with their authentic nature consistently report higher client satisfaction, better health outcomes, and greater personal fulfillment. They discover that honoring their empathetic gifts within sustainable structures doesn't compromise their service—it enhances it.
The choice facing every practitioner is ultimately simple: continue building a business that contradicts everything you teach about wellness, or discover how to align your practice with your authentic nature. Your clients need you healthy. Your family needs you present. Your purpose needs you sustainable.
The world needs healers who model the regenerative principles they teach. The empathy trap is real, but it is not permanent. With awareness, intention, and proper support, it becomes a doorway to practices that nourish rather than deplete, inspire rather than exhaust, and demonstrate that caring for others and caring for yourself are not opposing forces but complementary expressions of the same healing wisdom.
Research Methodology and Data Foundation
The findings presented in this analysis emerge from comprehensive research conducted by Stealth Dog Labs using proprietary technology that analyzes language patterns to quantify burnout risk, developmental mindset, and psychological stress indicators across professional populations.
Our dataset encompasses over 100 million professional profiles, with specific focus on healthcare practitioners, alternative medicine providers, and wellness professionals. The analysis employed Stealth Dog Labs' advanced algorithms that identify invisible metrics—psychological and behavioral patterns that predict performance outcomes months before they appear in traditional business or health indicators.
The technology works by analyzing communication patterns, language complexity, and psycholinguistic markers that correlate with specific developmental stages (using the Torbert Action Logic framework), empathy levels, and burnout trajectories. Unlike conventional surveys or self-reporting mechanisms, this approach captures unconscious patterns that individuals might not recognize or accurately report about themselves.
The Self-Martyrdom Complex scoring system represents a breakthrough in quantifying previously unmeasurable psychological patterns. By analyzing how individuals describe their work relationships, boundary management, and service motivation, the technology can predict burnout risk with remarkable accuracy—often 12-18 months before traditional indicators would detect problems.
This research represents the largest-scale analysis of practitioner burnout patterns ever conducted, made possible by Stealth Dog Labs' unique ability to process vast amounts of professional data while identifying subtle psychological patterns that remain invisible to conventional assessment methods.
For more information about Stealth Dog Labs' proprietary technology and research methodology, visit www.stealthdog.com.